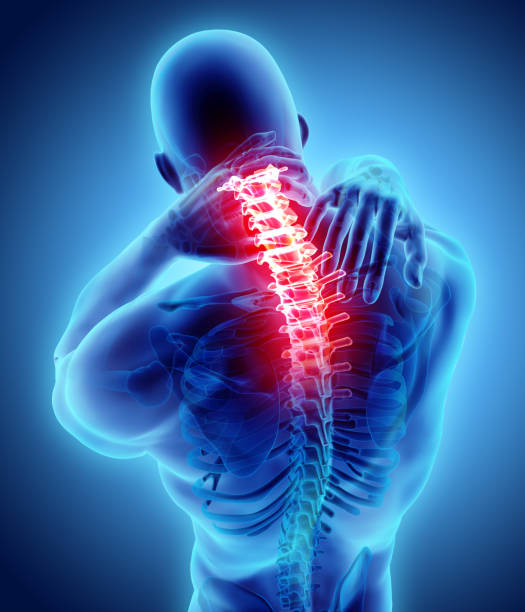
Have you ever wondered how long it takes for your body to heal after an injury? Understanding the healing process is crucial for managing pain and optimizing recovery. It’s not just about treating the symptoms – it’s about effectively managing the tissues involved to not only help you cope with and treat your […]
How Long Does it Take to Heal?